DRY EYE EXAMINATION AND TREATMENT
Dry Eye Examination
Dry eye disease is a multifactorial disease. The optometrist will conduct a thorough case history and examination to determine the cause and extent of your dry eye disease. Questions about your health, allergies, diet, and medication including eye drops and supplements, and lifestyle will be asked. A questionnaire about your symptoms will also be conducted to yield a better understanding of how dry eye disease is affecting you. These well-designed questionnaires are quick to conduct and are designed to reduce any bias as they offer no cues.

The following are some of the tests that may be conducted:
Staining dye tests such as Lissamine (green dye) and Sodium Fluoroscein (yellow-orange dye) – this helps the optometrist see the ocular surface for damage and dying cells. The ocular surface comprises of the corneas, conjunctivae and lid margins.
Phenol red thread test and Schirmer tear test – this is used to determine if aqueous production is adequate or not. The Phenol red thread test uses a pH-sensitive dye strip and takes 15 seconds to perform. The Schirmer test uses paper blotting strips and takes 5 minutes to perform.
Slit lamp examination/biomicroscopy – to look at tear instability, blinking rate, condition of eyelid margins, presence of debris on lashes, presence of sties, amount of inflammation on the ocular surface and lids
Lacrimal lavage – this test is performed if the patient has a constant ‘wet’ eye, to assess for potential damage to the punctal (drainage) ducts of the eyes.
I-pen – this electronic diagnostic device masures the patient’s tear osmolarity (i.e. the concentration of salt in the tear film). It is a quick and simple test to perform. A single use sensor tip is bathed in the tear film of the lower lid for about two seconds to obtain a reading.
Non invasive tests performed on an advance technology machine called Oculus Keratograph5 – This unit is able to tests for evaporation time, degree of redness on the conjunctiva, amount of tears present on the lower lid, lipid layer assessment and most importantly meibography. Meibography is an infrared scan of the meibomian (oil) glands that are responsible for providing the oil component in our tears.
InflammaDry – this is a test to ascertain the presence of MMP-9, a molecule known to cause inflammation.
Meibomian gland evaluator – this small device is used to assess the quality of meibomian oil that gets expressed from a standard deliberate blink.
At the end of the dry eye assessment, the optometrist will discuss the following:
Advice on which eye drops are suitable for you. Some may be available over the counter whilst others may be prescribed.
Advice on diet and the environment.
Products that can provide you with relief such as moisture chamber goggles, warming devices for home use.
Advance in-office dry eye treatments – Intense Pulse Light (IPL), Lipiflow, Rexon-Eyes.
Dry Eye Treatment
Treatment of dry eye disease is based on the underlying cause and its severity. At the end of the dry eye examination, the optometrist will present a personalised treatment plan. It is important to remember that dry eye is a chronic disease and it cannot be cured. Ongoing management and treatment can offer improvement in your quality of life, as well as slow down the disease progression. Untreated cases can be debilitating due to significant discomfort and blurry vision. It may also result in corneal erosions, ulcers and scars but rarely will cause vision loss.
Lifestyle changes:
Use of regular lubricants. Not all over the counter eye drops are the same. The optometrist will recommend suitable products for you.
Reduce screen time where possible.
Perform regular blinking exercises during the day.
Avoid environments that are dusty, smoky, or have chemical fumes.
Avoid sitting in front of vents or beneath fans, at work and at home.
Invest in a good humidifier or make your own by placing bowls of water in the room.
Invest in a good pair of wrap-around polarised sunglasses.
Reduce contact lens wearing time.
Use commercial eyelid warming compresses and follow with gentle lid massage regularly.
Use commercial lid and lash cleaners to maintain good eyelid hygiene.
Dietary changes – drink more water, take less caffeinated drinks and consume foods high in Omega-3 fatty acids.
Be aware that certain prescribed medications can increase dry eye symptoms.
Get plenty of sleep.
What optometrists and ophthalmologists can do:
Prescribe eyedrops such as steroid drops and cyclosporine to reduce inflammation.
Prescribe dry eye supplements such as Lacritec and DryEyeForte. These are high in Omega-3 fatty acids.
Fit special contact lenses such as sclera contact lenses and bandage contact lenses.
Prescribe Doxcycline tablets or topical Azithromycin – These medications have antibiotic and anti-inflammatory properties and have been shown to be effective in treating dry eye disease.
Recommend Optimel (Manuka honey) eye drops and gel drops – These products have natural antibiotic and anti-inflammatory properties.
Punctal plugs to help retain tears on the ocular surface by blocking some of the drainage outlets. These plugs are not permanent and can be removed. Cauterisation of the punctal ducts is a permanent procedure, performed by ophthalmologists.
Autologous blood serum eyedrops – ASED are eye drops are manufactured from a patient’s own blood. They contain specific nutrients and growth factors that nourish and heal the ocular surface. They are prescribed for patients with severe ocular surface disorders.
In-office Blephasteam – this simple procedure is used for patients with mild meibomian gland disease. It involves wearing a warming goggle set at a constant temperature targeted to melt blocked oil within the glands for ten minutes. Following this, the optometrist performs manual meibomian gland expression to release any blocked meibum/oil within the orifices. Once the glands are unblocked, normal meibum/oil can be released through normal blinking.
Types of Procedures for Dry Eye
How Rexon-Eye works:
Rexon Eye can be used for all types of dry eye disease, unlike IPL and Lipiflow which targets meibomian gland disease. This technology is based on using low-power high-frequency electric fields to regenerate tissues around the eyes. During the procedure, the patient wears the goggle device for 20minutes. Following this, whilst there is residual heat, the optometrist performs a meibomian gland expression to clear away any blocked ducts.
How IPL (Intense Pulse Light) works:
IPL works on three mechanisms. It uses visible light and infrared light flashes to target and seal off inflammatory blood vessels around the eyes. It helps stimulate the nerves of the meibomian glands, helping to restore their function. The heat that comes from these flashes is warm enough to kill harmful bacteria and mites around the eyes. The heat is also very effective at melting meibum blocked inside the ducts. Following this procedure, the optometrist will do a manual meibomian gland expression.
EYE-LIGHT Intense Pulse Light
IPL has become the mainstream treatment for dry eyes and as such, there are several IPL machines approved by the TGA. The Eye-Light IPL is unique in that it uses Optimal Power Energy (OPE) IPL to deliver thermal pulses that have a high degree of safety, effectiveness and accuracy. No gel is required due to its unique built-in cooling system in the IPL head unit. It treats a larger area with each pulse compared to other IPL machines due to its larger head design. The device is easy to use with no side effects and the patient will find the treatment procedure quick and comfortable.

Low Level Light Therapy (LLLT)
LLLT has been approved by the TGA as an effective treatment for dry eye disease. LLLT works by inducing photo-biomodulation in the cellular metabolism, to repair and regenerate damaged cells and improve cellular function. LLLT also has analgesic (pain management), aesthetic (anti-wrinkling) and anti-inflammatory effects. LLLT is also known as cold laser therapy. The light is absorbed by the body tissue, causing a reaction that releases heat in the process. As LLLT is athermal, there is no thermal risk to the patient.
LLLT machine uses three different masks. The most commonly used LED is the red, for the treatment of MGD dry eyes and styes. LLLT has been shown to be a more effective option especially in children with multiple styes, than prescribing oral antibiotics or referring them for surgery. The blue mask is used for treating Demodex blepharitis, by killing bacteria. Yellow is less commonly used by optometrists as their primary use is for post-surgical recovery.
It is a safe, pain-free, non-invasive and highly effective treatment approved for the use in adults and children. Unlike other dry eye treatment machines, there really is no contraindication for its use. The treatment does not require the patient to wear eye shields. As such, the greatest advantage over other treatment modalities is that the both the upper and the lower lids are targeted, improving treatment efficacy. The facial mask covers the eyes, the periorbital area and the upper cheek areas.
Patients are encouraged to close their eyes for a more relaxing experience and opening them during treatment is not harmful. The machine is easy to operate. The doctor simply selects the appropriate LED colour mask based on what condition is being treated. When treating meibomian gland dysfunction dry eye disease, the level of severity is inputted and the software will run the appropriate program.
The LLLT device can be used as a standalone treatment for dry eyes, or as an adjunct to IPL. Studies have shown superior effectiveness for treating dry eyes when therapies are combined than IPL alone. IPL when used with blue mask LLLT is also very effective at treating ocular and facial rosacea. These dermatological conditions are often seen in patients with dry eyes.


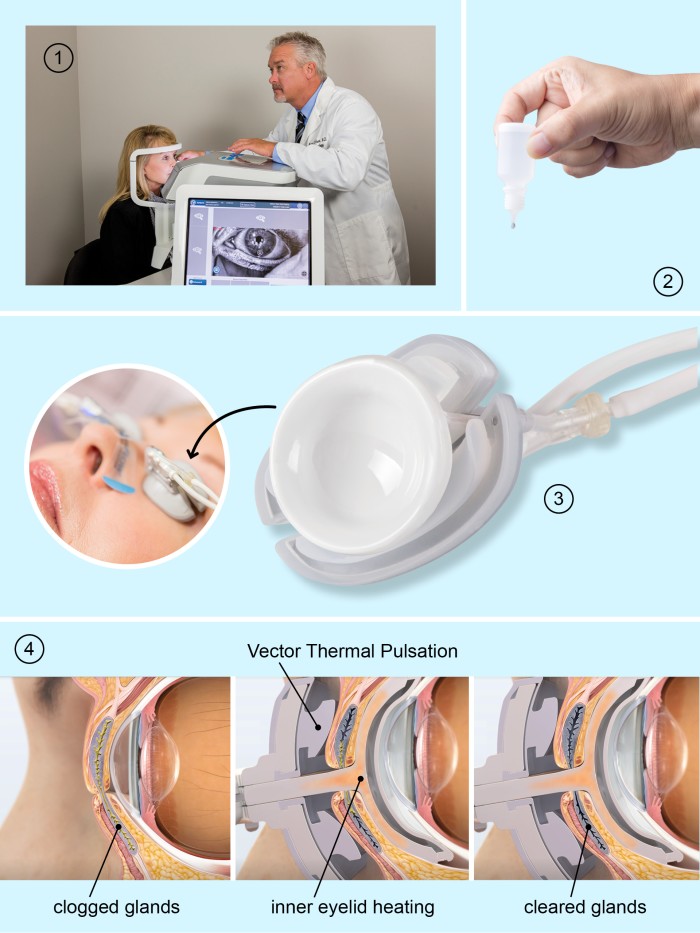
How Lipiflow works:
Lipiflow is an automated thermal pulsation system. The optometrist places a sterile dome-shaped cupping device over each eye. This unique design protects the cornea and holds both the top and bottom set of lids in place. This effective single 12minute procedure essentially combines warm compresses with gentle meibomian gland expression. performs a meibomian gland expression to clear away any blocked ducts.
Image source.
Procedural Fees:
IPL: Single treatment $200 (4 treatment package $750)
Rexon-Eyes: Single treatment $200 (4 treatment package $750)
- Low-level light therapy: Single treatment $200 (4 treatment package $750)
Lipiflow: Single treatment $750
